Mental Health: It took a global pandemic to rethink our ‘put on a brave face’ approach

By Adrita Bhattacharya-Craven
Across the world, people have been faced with increased feelings of loneliness, anxiety and uncertainty, as well as dealing with bereavements and burnouts over the past 18 months. In the U.S., over 40% of adults reported a worsening of their mental health during the COVID-19 pandemic, often associated with problems sleeping, increased alcohol consumption, substance misuse and deteriorating physical health.[1] In the EU, 64% of young people under the age of 34 were reported to be at risk of depression during the spring 2020 lockdowns.[2] Prolonged periods of social restrictions, isolation and insecurities related to loss of income have led many to experience poor or deteriorating mental health and exposed a growing and hitherto silent epidemic.
Global government expenditure on mental healthcare stands at a meagre USD 2.5 per capita, with particularly stark underinvestment in low- and middle-income countries.
As of 2017, the Institute for Health Metrics Evaluation estimated over 970 million people globally suffer from mental health disorders,[3] with a significant economic toll – loss of productivity is estimated at USD 1 trillion per year.[4] Yet, mental healthcare has remained a ‘Cinderella service’ with global government expenditure standing at a meagre USD 2.5 per capita, and particularly stark underinvestment in low- and middle-income countries.[5] COVID-19 has not only placed immense pressure on mental well-being, it has also exacerbated an already widespread mental health crisis characterised by inadequate funding and workforce shortages for mental health services. The time is now ripe to acknowledge the true scale of the vulnerabilities and risks poor mental health poses to our society. 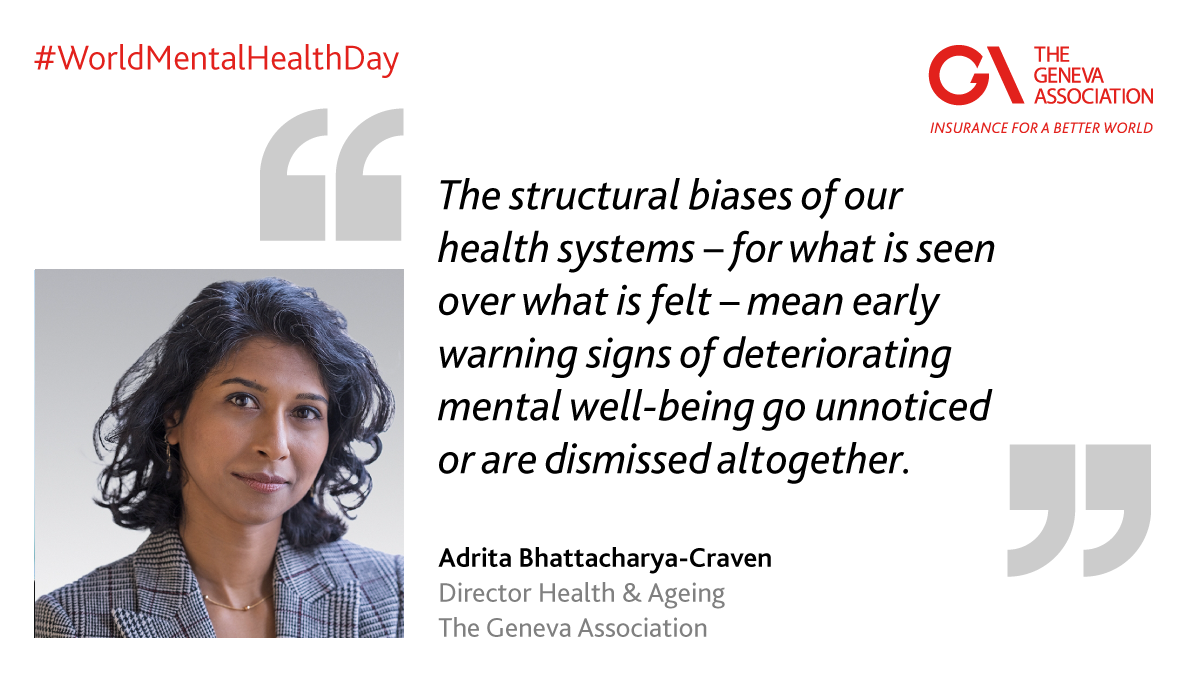
Historically, health payers (including voluntary health insurers) and health service providers have compartmentalised physical and mental health. In reality, however, complex comorbidities have blurred the lines between the two. There is evidence to suggest that the state of emotional and social well-being is inextricably linked with physical health outcomes, with as much as 29% heightened risk of coronary heart disease and 32% increased risk of stroke associated with poor mental well-being.[6] Other studies have established links between non-communicable diseases such as diabetes and cancer and mental health problems.[7] Nevertheless, the structural biases of our health systems for what is seen (i.e. a physical ailment) over what is felt mean early warning signs of deteriorating mental well-being go unnoticed or are dismissed altogether. This has been the case for decades and has in turn undermined access to mental health services and fuelled the deep-seated social stigma associated with mental illness.
Insurers should appreciate the different avenues through which mental well-being can be bolstered and disorders can be managed by offering comprehensive support that is devoid of stigma.
The COVID-19 crisis has given societies, governments and the private sector a rare opportunity to more effectively address the problem. While strengthening mental health services should remain at the heart of any solution, the approach will have to be multifaceted. Insurers should appreciate the different avenues through which mental well-being can be bolstered and disorders can be managed by offering comprehensive support that is devoid of stigma.[8] This could mean insurers encouraging public and private employers to address mental well-being at the workplace, establishing warning signs for potential triggers, such as an accident, bereavement or a critical illness episode. Insurers could design products, such as personalised health and social care plans, that incorporate structured loneliness assessments or community-support services to actively break down social isolation, especially among the elderly and vulnerable groups.[9]
It also requires doing away with the rigid lines between life, health and property and casualty insurance and instead treating the customer journey as a holistic experience. This not only warrants organisational integration but, more importantly, a bold acknowledgement from the industry that poor mental health is a risk for all. It not only worsens morbidity and mortality; its presence undermines productivity across sectors.
Implicit in the notion of insurance is the idea of ‘having peace of mind’ in order to protect people at their most vulnerable moments – triggered either by a material or a non-material loss. Insurers now have a golden opportunity to embrace that phrase in every sense of the word, to make communities and economies more resilient as we navigate our way out of this crisis.
References
[1] https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/
[2] https://www.eurofound.europa.eu/sites/default/files/ef_publication/field_ef_document/ef21064en.pdf
[3] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6227754/pdf/main.pdf
[4] https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(20)30432-0/fulltext
[5] https://www.who.int/publications/i/item/9789241514019
[6] https://heart.bmj.com/content/102/13/1009
[7] https://www.bmj.com/content/364/bmj.l295
[8] https://www.swissre.com/reinsurance/life-and-health/l-h-risk-trends/mind-matters.html
[9] https://www.commonwealthfund.org/blog/2020/solutions-around-world-tackling-loneliness-and-social-isolation-during-covid-19